Publication
- Title: Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome
- Acronym: Not reported (commonly referred to as the ARDSNet low tidal volume / “ARMA” trial)
- Year: 2000
- Journal published in: The New England Journal of Medicine
- Citation: Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301-1308.
Context & Rationale
-
Background
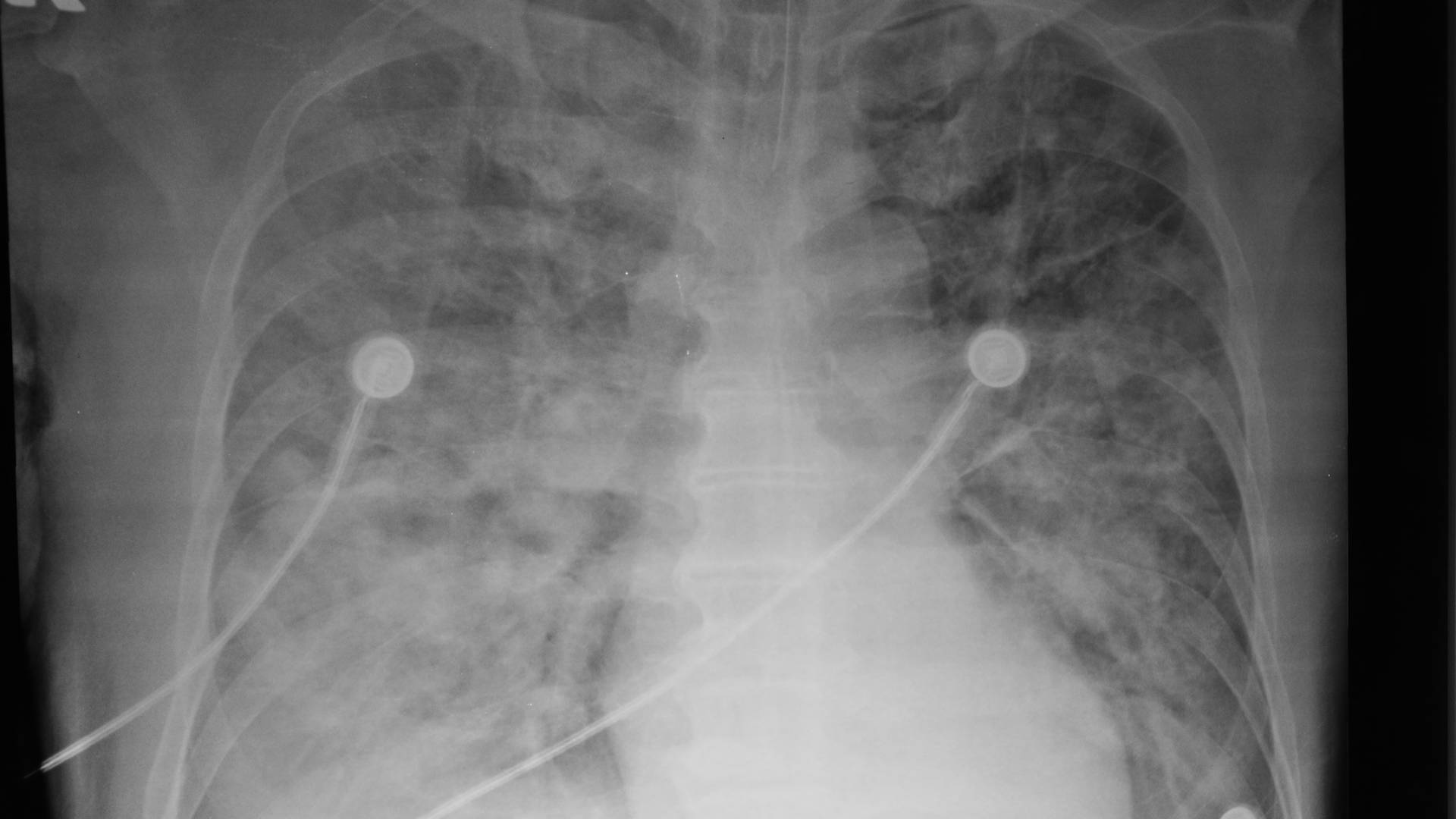
- By the mid-1990s, ventilator-induced lung injury (volutrauma/barotrauma and “biotrauma”) was increasingly recognised as a plausible, iatrogenic amplifier of acute lung injury.
- Common practice used comparatively large tidal volumes (often 10–15 mL/kg), with permissive plateau pressures that could exceed what is now considered safe.
- Small randomised trials of “protective” strategies (lower tidal volumes, higher PEEP) produced conflicting results and were heterogeneous in co-interventions, limiting confidence in causality.
- A definitive, adequately powered multicentre trial was needed to determine whether limiting tidal volume and plateau pressure improves patient-centred outcomes in ALI/ARDS.
-
Research Question/Hypothesis
- In intubated adults with acute lung injury/ARDS, does a ventilation strategy targeting lower tidal volumes and lower plateau pressures reduce mortality and increase ventilator-free days compared with “traditional” tidal volumes?
-
Why This Matters
- Mechanical ventilation is universal supportive therapy in ARDS; even modest improvements in ventilator strategy could have large absolute public-health impact.
- Demonstrating benefit would justify a paradigm shift from “normalising” gas exchange to prioritising lung protection, with downstream effects on sedation, acid–base management, and adjunctive therapies.
- Conversely, demonstrating no benefit (or harm) would prevent widespread adoption of permissive hypercapnia and lower tidal volume strategies with potential physiological trade-offs.
Design & Methods
- Research Question: In adults with ALI/ARDS receiving mechanical ventilation, does targeting a lower tidal volume (with a plateau pressure ≤30 cm H2O) improve survival and ventilator-free days compared with traditional tidal volumes (plateau pressure ≤50 cm H2O)?
- Study Type: Randomised, multicentre, parallel-group, investigator-initiated ARDS Network trial conducted in 10 university-affiliated centres (United States); open-label ventilation strategy with protocolised co-interventions.
- Population:
- Setting: ICU patients requiring invasive mechanical ventilation.
- Core inclusion criteria: Intubated and mechanically ventilated; acute onset; bilateral infiltrates consistent with pulmonary oedema; PaO2/FiO2 ≤300 (ALI) and ≤200 (ARDS); no clinical evidence of left atrial hypertension (pulmonary-artery wedge pressure ≤18 mm Hg if measured).
- Key exclusions (selected): Age <18 years; pregnancy; severe chronic respiratory disease; intracranial hypertension; neuromuscular disease impairing spontaneous breathing; bone marrow transplant; burns >30% total body surface area; weight >1 kg per cm of height; other conditions with an estimated 6‑month mortality >50%.
- Intervention:
- Ventilation strategy: Initial tidal volume 6 mL/kg predicted body weight (PBW), with a plateau pressure target ≤30 cm H2O; adjustments permitted per protocol (including tidal volume range 4–8 mL/kg PBW depending on plateau pressure and pH management).
- Gas-exchange targets: PaO2 55–80 mm Hg or SpO2 88–95% using a protocolised FiO2/PEEP table.
- Ventilation management: Increased respiratory rate to offset reduced tidal volume; permissive hypercapnia accepted within protocolised pH thresholds.
- Weaning: Daily assessment for discontinuation of ventilation using prespecified criteria.
- Comparison:
- Ventilation strategy: Initial tidal volume 12 mL/kg PBW with plateau pressure limit ≤50 cm H2O; protocolised adjustments permitted.
- Gas-exchange targets and weaning: Same PaO2/SpO2 goals, FiO2/PEEP table, and weaning approach as the intervention arm.
- Blinding: Unblinded (ventilator settings could not be masked); primary outcomes were objective, but unblinded management could influence co-interventions.
- Statistics: Power calculation / target effect size / required sample size not reported in the published manuscript; group sequential monitoring with interim analyses using the Lan–DeMets alpha-spending approach with O’Brien–Fleming boundaries; primary analyses were intention-to-treat.
- Follow-Up Period: Daily assessment through day 28; survival and breathing status assessed to day 180.
Key Results
This trial was stopped early. Recruitment stopped after enrolment of 861 patients at the fourth interim analysis because mortality was lower in the lower tidal volume group (P=0.005 at interim; stopping boundary 0.023).
| Outcome | Lower tidal volume strategy | Traditional tidal volume strategy | Effect | p value / 95% CI | Notes |
|---|---|---|---|---|---|
| Death before discharge home with unassisted breathing | 31.0% (134/432) | 39.8% (171/429) | Difference 8.8 percentage points | 95% CI 2.4 to 15.3 percentage points; P=0.007 | Primary outcome |
| Ventilator-free days (to day 28) | 12 ± 11 days | 10 ± 11 days | Not reported | P=0.007 | Defined as days alive and breathing without assistance to day 28 |
| Days without failure of any nonpulmonary organ system (to day 28) | 15 ± 11 days | 12 ± 11 days | Not reported | P=0.006 | Nonpulmonary organ failure defined a priori (e.g., shock, renal failure) |
| Breathing without assistance at day 28 | 65.7% (284/432) | 55.0% (236/429) | Not reported | P=0.009 | Secondary outcome |
| Barotrauma | 10% (43/432) | 11% (47/429) | Not reported | P=0.43 | Pneumothorax, pneumomediastinum, pneumoperitoneum, subcutaneous emphysema, or air cysts |
| Death at day 180 | 34.7% (150/432) | 42.5% (182/429) | Not reported | P=0.007 | Vital status known for all but 9 patients |
| Breathing without assistance at day 180 | 71.9% (311/432) | 62.0% (266/429) | Not reported | P=0.003 | Secondary outcome |
- Protocol separation was substantial: mean tidal volume on days 1–3 was 6.2 ± 0.8 mL/kg PBW vs 11.8 ± 0.8 mL/kg PBW; mean plateau pressure was 25 ± 6 cm H2O vs 33 ± 8 cm H2O.
- The lower tidal volume strategy resulted in higher PaCO2 and slightly lower pH early in the course (e.g., day 1 PaCO2 44 ± 11 mm Hg vs 40 ± 10 mm Hg; pH 7.38 ± 0.07 vs 7.41 ± 0.07).
- Benefit was durable to day 180, without an observed reduction in barotrauma.
Internal Validity
- Randomisation and allocation concealment: Central randomisation via an automated telephone system; allocation concealment likely robust; factorial co-randomisation to ketoconazole/lisofylline balanced by design.
- Completeness of follow-up: 861 randomised (432 vs 429); 180‑day vital status unknown for 9 patients; primary in-hospital outcomes were essentially complete.
- Performance/detection bias: Open-label ventilation strategy introduces risk of differential co-interventions; primary outcomes (mortality, ventilator-free days) are objective and less prone to assessment bias.
- Baseline comparability: Groups were well matched (e.g., age 51 ± 17 vs 52 ± 18 years; APACHE III 81 ± 28 vs 84 ± 28; PaO2/FiO2 138 ± 64 vs 134 ± 58; baseline plateau pressure 33 ± 10 vs 33 ± 11 cm H2O).
- Protocol adherence and separation of the variable of interest:
- Tidal volume (mL/kg PBW): day 1: 6.5 ± 0.9 vs 11.8 ± 0.8; day 2: 6.3 ± 0.9 vs 11.7 ± 0.8; day 3: 6.2 ± 0.9 vs 11.7 ± 0.8; day 4: 6.1 ± 0.9 vs 11.6 ± 0.8 (P<0.001 for each day).
- Plateau pressure (cm H2O): day 1: 25.1 ± 6.2 vs 31.8 ± 7.8; day 2: 24.0 ± 6.0 vs 30.8 ± 8.1; day 3: 23.7 ± 6.0 vs 30.5 ± 7.6; day 4: 23.4 ± 6.0 vs 29.9 ± 7.6 (P<0.001 for each day).
- Co-intervention signal (PEEP): day 1: 8.3 ± 3.2 vs 7.3 ± 3.0 (P<0.001); day 3: 8.6 ± 3.3 vs 7.2 ± 3.2 (P<0.001).
- Physiological consequences (permissive hypercapnia): day 1 PaCO2 44 ± 11 vs 40 ± 10 mm Hg (P<0.001); day 1 pH 7.38 ± 0.07 vs 7.41 ± 0.07 (P<0.001).
- Timing: Randomisation occurred at the time ALI/ARDS criteria were met (acute onset) and while patients were invasively ventilated; this aligns with the biological rationale of preventing early ventilator-induced injury.
- Statistical rigour: Prespecified group sequential monitoring with conservative O’Brien–Fleming stopping boundaries; early stopping may inflate effect estimates, but the decision was rule-based and supported by consistent day‑180 outcomes.
Conclusion on Internal Validity: Overall, internal validity appears moderate-to-strong given concealed randomisation, objective outcomes, and clear protocol separation, but is tempered by the open-label design, small between-group differences in PEEP, and early stopping.
External Validity
- Population representativeness: Typical adult ALI/ARDS case-mix in academic ICUs (baseline PaO2/FiO2 ~135–140; baseline plateau pressure ~33 cm H2O), but excludes several clinically important subgroups.
- Key exclusions affecting generalisability: Severe chronic respiratory disease, intracranial hypertension, extreme obesity (weight >1 kg/cm height), major burns, and high competing risk of death (>50% at 6 months) limit extrapolation to these populations.
- Applicability across systems: Implementation is feasible in most ventilated ICU environments, but requires accurate height measurement, PBW calculation, and staff familiarity with permissive hypercapnia and plateau pressure measurement.
- Resource-limited settings: The core intervention (tidal volume/plateau pressure targets) is low-cost, but adherence may be constrained by staffing, monitoring capacity, and limited availability of advanced ventilator modes/alarms.
Conclusion on External Validity: Findings are highly generalisable to adult ALI/ARDS patients receiving invasive ventilation in well-resourced ICUs, but should be extrapolated cautiously to excluded groups (notably intracranial hypertension and severe chronic lung disease) and to contexts with limited monitoring/training.
Strengths & Limitations
- Strengths:
- Large multicentre randomised trial with central allocation concealment within an established critical care network.
- Clear, protocolised ventilator management with large, quantifiable separation in tidal volume and plateau pressure.
- Clinically meaningful, objective primary outcomes with follow-up to 180 days.
- Consistent directionality across mortality and ventilator/organ-failure–free outcomes.
- Limitations:
- Unblinded intervention with potential for differential co-interventions (including small but statistically significant differences in PEEP early after randomisation).
- Early stopping for benefit increases the risk of overestimating effect size and limits precision.
- Control strategy (12 mL/kg PBW; plateau pressure limit ≤50) may be viewed as injurious by contemporary standards, complicating interpretation as “optimisation” vs “harm avoidance”.
- Power calculation and original target sample size were not reported in the manuscript, limiting transparency around planned operating characteristics.
Interpretation & Why It Matters
-
Practice-changing effectDemonstrated that a lung-protective strategy (6 mL/kg PBW; plateau pressure ≤30 cm H2O) improves survival and increases ventilator-free days compared with traditional tidal volumes.
-
Mechanistic implicationSupports the concept that ventilator-induced lung injury is not merely a theoretical concern but a modifiable determinant of outcomes in established ALI/ARDS.
-
Implementation nuanceRequires accurate PBW calculation (height/sex based), routine plateau pressure measurement, and comfort with permissive hypercapnia within a structured safety framework.
-
Research legacyEstablished a standardised ventilatory “platform” for subsequent ARDS trials (PEEP, recruitment, prone positioning, neuromuscular blockade, ECMO), improving comparability of later evidence.
Controversies & Subsequent Evidence
- The accompanying editorial framed the trial as a decisive culmination of the lung-protective ventilation debate and underscored the biological plausibility of iatrogenic injury from overdistension and excessive airway pressures.1
- Correspondence emphasised that the comparison was between bundled ventilation strategies (including modestly higher PEEP and more permissive hypercapnia in the lower tidal volume arm) rather than tidal volume in isolation, raising mechanistic uncertainty about which component(s) mediated benefit.2
- The control arm (12 mL/kg PBW with plateau pressure ≤50 cm H2O) has been criticised as potentially injurious by modern standards; this reframes the observed benefit as avoidance of harm rather than proof that 6 mL/kg is uniquely optimal.
- Early stopping for benefit can exaggerate effect size; however, stopping used conservative O’Brien–Fleming boundaries and the mortality difference persisted to day 180.
- Subsequent society guidance consistently recommends low tidal volume ventilation (typically 4–8 mL/kg PBW) with plateau pressure limitation as foundational ARDS management, embedding ARMA’s core findings into practice recommendations.3
- Large international observational data show that adherence to lung-protective ventilation remains imperfect and varies widely, implying ongoing implementation gaps even after landmark efficacy evidence.4
Summary
- In 861 adults with ALI/ARDS, a lower tidal volume strategy (6 mL/kg PBW; plateau pressure ≤30 cm H2O) reduced mortality compared with a traditional tidal volume strategy (12 mL/kg PBW; plateau pressure ≤50 cm H2O).
- The trial was stopped early at a prespecified interim analysis because of a mortality benefit, with durable benefit to 180 days.
- Lower tidal volumes increased ventilator-free days and days without nonpulmonary organ failure, suggesting both respiratory and systemic benefit.
- Physiological trade-offs were expected and observed (higher PaCO2, slightly lower pH), but did not translate into excess barotrauma.
- ARMA established lung-protective ventilation as the default “platform” for modern ARDS care and subsequent trials.
Overall Takeaway
ARMA provided definitive multicentre evidence that limiting tidal volume and plateau pressure improves survival in ALI/ARDS, anchoring lung-protective ventilation as foundational critical care practice. Its influence extends beyond ARDS, shaping a broader safety culture in mechanical ventilation and providing a common ventilatory platform for subsequent ARDS therapeutics trials.
Overall Summary
- Lower tidal volume, plateau-pressure–limited ventilation reduces mortality and increases ventilator-free days in ALI/ARDS.
- Physiological consequences (permissive hypercapnia) are manageable within protocolised safety thresholds.
- Despite strong efficacy evidence, real-world uptake varies—implementation remains a key quality target.
Bibliography
- 1.Tobin MJ. Culmination of an era in research on the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1360-1361.
- 2.Laffey JG, Kavanagh BP. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;343(11):812-814.
- 3.Fan E, Del Sorbo L, Goligher EC, Hodgson CL, Munshi L, Walkey AJ, et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(9):1253-1263.
- 4.Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788-800.