Publication
- Title: Recombinant factor VIIa versus placebo for spontaneous intracerebral haemorrhage within 2 h of symptom onset (FASTEST): a multicentre, double-blind, randomised, placebo-controlled, phase 3 trial
- Acronym: FASTEST
- Year: 2026
- Journal published in: The Lancet
- Citation: Broderick JP, Naidech AM, Elm JJ, et al. Recombinant factor VIIa versus placebo for spontaneous intracerebral haemorrhage within 2 h of symptom onset (FASTEST): a multicentre, double-blind, randomised, placebo-controlled, phase 3 trial. Lancet. 2026; published online Feb 4.
Context & Rationale
-
Background
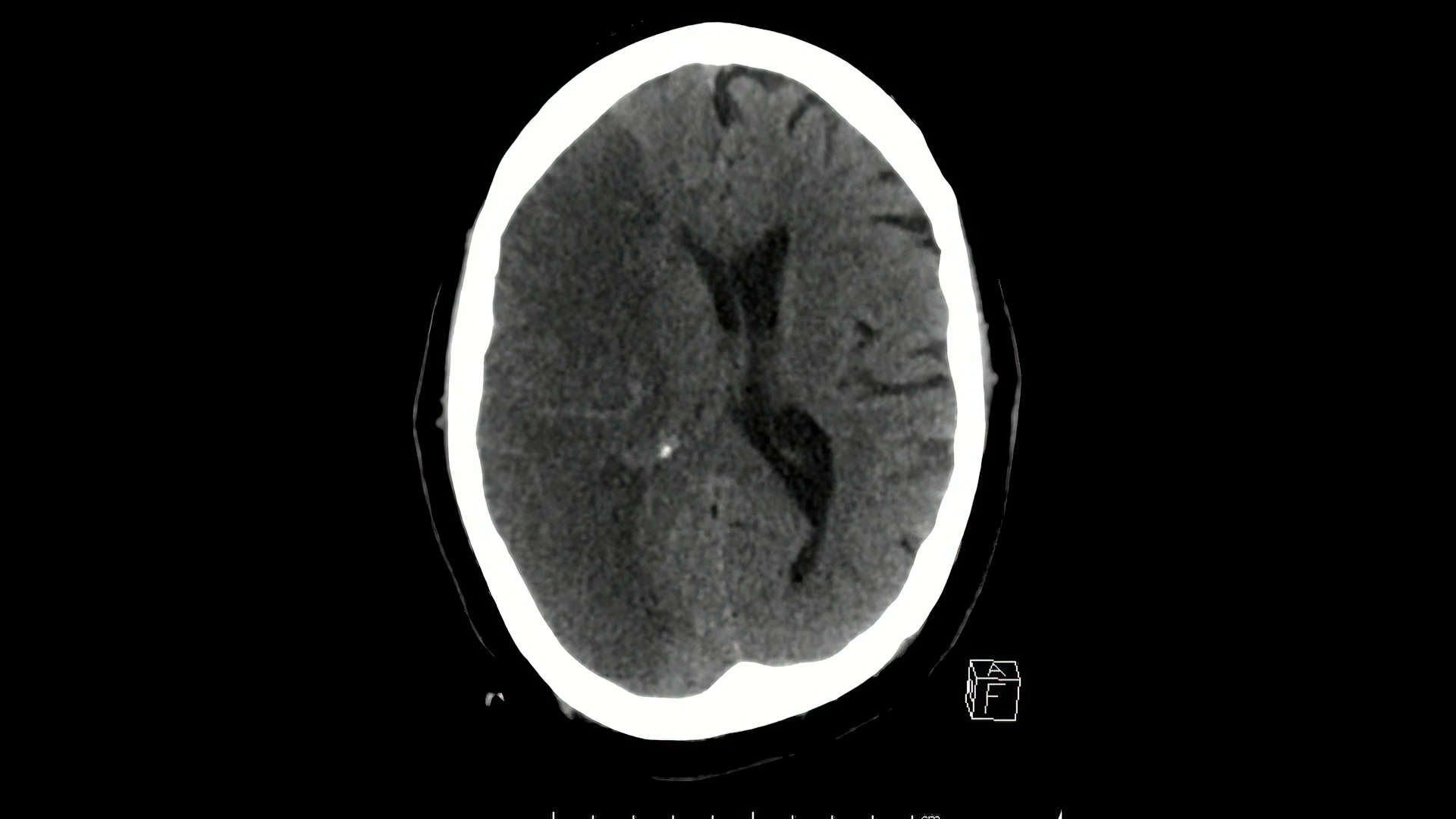
- Spontaneous intracerebral haemorrhage (ICH) has high early mortality and disability, with outcome strongly related to initial haematoma volume and subsequent expansion.
- Most haematoma expansion occurs within the first 2–3 hours after symptom onset, creating a narrow window for haemostatic intervention.
- Recombinant factor VIIa (rFVIIa) had previously reduced haematoma growth but did not improve functional outcomes when given within 4 hours, and increased arterial thromboembolic events, leading to recommendations against routine use.1
- Post-hoc analyses suggested potential benefit in ultra-early treatment and in patients with imaging/clinical features indicating ongoing bleeding (e.g., CT angiography spot sign; shorter onset-to-treatment time).2
-
Research Question/Hypothesis
- Does intravenous rFVIIa (80 μg/kg, max 10 mg) given within 2 hours of onset/last known well improve 180-day functional outcome after spontaneous ICH compared with placebo, while reducing ICH/IVH growth?
-
Why This Matters
- If ultra-early haemostasis could convert a biological effect (reduced expansion) into functional recovery, this would be a paradigm-shifting acute therapy for ICH, analogous to time-critical reperfusion in ischaemic stroke.
- Conversely, definitive neutral or harmful findings would prevent off-label use of a potent procoagulant with meaningful thromboembolic risk.
Design & Methods
- Research Question: In adults with spontaneous ICH treatable within 2 hours, does rFVIIa improve 180-day functional outcome compared with placebo, and what are the effects on haematoma growth and thromboembolic harm?
- Study Type: Multicentre, international, double-blind, randomised, placebo-controlled, adaptive phase 3 trial; emergency enrolment pathways including mobile stroke units; ICU/stroke-unit level care after treatment.
- Population:
- Adults 18–80 years with spontaneous ICH on baseline CT, ICH volume 2–60 mL, Glasgow Coma Scale ≥8, and treatable within 120 minutes of symptom onset/last known well.
- IVH permitted only if limited: <2/3 of one lateral ventricle or <1/3 of both lateral ventricles.
- Key exclusions included: secondary/structural causes (e.g., trauma, aneurysm/AVM), anticoagulant use within 7 days, pre-existing disability (mRS >2), brainstem haemorrhage (cerebellar allowed), symptomatic thromboembolic/vaso-occlusive disease within 90 days (e.g., cerebral infarction, MI, PE/DVT, unstable angina), and planned withdrawal of care.
- Intervention:
- rFVIIa 80 μg/kg (maximum 10 mg) administered intravenously over 2 minutes as soon as possible and within 2 hours of onset/last known well.
- Comparison:
- Matching placebo (identical solvent/process), same volume and 2-minute IV administration.
- Blinding: Double-blind (participants, clinicians, outcome assessors, and analysts); interim analyses conducted by an unmasked statistician and DSMB independent of trial conduct.
- Statistics: Sample size 388 per group to detect a 10% absolute increase in mRS 0–2 (assumed 40% to 50%) with 80% power at two-sided α=0.05; inflated to 860 total for ~10% missing and interim analysis; adaptive sample size re-estimation/enrichment planned (maximum 1330) with futility stopping (conditional power <0.20) and superiority stopping via O’Brien–Fleming boundaries; primary analysis by ordinal logistic regression adjusted for age, baseline ICH volume, baseline IVH volume, and pre-stroke mRS (intention-to-treat).
- Follow-Up Period: Imaging at 24 hours (or earlier if surgery required); clinical follow-up at days 30, 90, and 180.
Key Results
This trial was stopped early. Stopped at the second preplanned interim analysis for futility after 626 of planned 860 participants were randomised (conditional power <0.20; reported as <1% under observed trend).
| Outcome | rFVIIa (n=328) | Placebo (n=298) | Effect | p value / 95% CI | Notes |
|---|---|---|---|---|---|
| Primary: mRS at 180 days (0–2 / 3 / 4–6) | 46% / 24% / 30% | 45% / 26% / 30% | Adj common OR 1.09 | 95% CI 0.79 to 1.51; P=0.61 | Ordinal logistic regression adjusted for age, baseline ICH volume, baseline IVH volume, pre-stroke mRS |
| mRS at 90 days (0–2 / 3 / 4–6) | 40% / 18% / 42% | 38% / 19% / 43% | Adj common OR 1.13 | 95% CI 0.82 to 1.56; P=0.87 | Secondary efficacy endpoint |
| ICH growth baseline→24 h (mL) | 1.9 ± 7.0 | 5.5 ± 13.7 | Adj mean diff −3.68 mL | 95% CI −5.40 to −1.94; P=0.0011 | Secondary mechanistic endpoint |
| ICH+IVH growth baseline→24 h (mL) | 2.2 ± 8.4 | 7.4 ± 19.6 | Adj mean diff −5.23 mL | 95% CI −7.64 to −2.82; P=0.0011 | Secondary mechanistic endpoint |
| Primary safety: life-threatening thromboembolic events within 4 days | 15 (<5%) | 4 (1%) | RR 3.41 | 95% CI 1.14 to 10.15; P=0.020 | Acute MI, acute cerebral infarction, or acute PE |
| All-cause mortality by 180 days | 20 (6%) | 22 (7%) | RR 0.83 | 95% CI 0.46 to 1.48 | Not statistically different |
- Ultra-early rFVIIa reduced ICH (and ICH+IVH) expansion by ~3.7–5.2 mL but did not improve 180-day functional outcome.
- Life-threatening thromboembolic events within 4 days were increased (RR 3.41).
- Signals of potential benefit were observed in small, prespecified “ongoing bleeding” subgroups (treatment <90 min; CTA spot sign), but the overall result was neutral and the trial stopped early for futility.
Internal Validity
- Randomisation and allocation concealment: Simple 1:1 randomisation using lowest-numbered pre-randomised kit at each site, enabling rapid enrolment; kit preparation/labelling separated from enrolment teams, supporting concealment.
- Early stopping: Stopped for futility after 626/860 randomised, reducing precision and power for modest functional effects (particularly within subgroups) and increasing the risk of over-interpreting subgroup signals.
- Dropout/exclusions and follow-up: Trial profile indicates near-complete treatment delivery (placebo 297/298 received full treatment; rFVIIa 328/328 received full treatment); losses to follow-up at day 180 were small (placebo: 3 lost + 3 withdrew; rFVIIa: 4 lost + 1 withdrew), with multiple imputation for missing mRS.
- Performance/detection bias: Double blinding and centrally read imaging reduce biased co-interventions and outcome assessment; functional outcome measured using a structured tool (Rankin Focused Assessment Tool).
- Protocol adherence and separation: Intervention was a single 2-minute IV administration; separation was clear. Co-interventions were guideline-based and not protocolised beyond required acute BP management (target SBP 140 mm Hg).
- Baseline balance: Core prognostic variables were similar (age ~61, baseline ICH volume ~17 mL, NIHSS median 13); a higher proportion underwent CTA in placebo (85%) vs rFVIIa (78%), which could influence subgroup ascertainment (spot sign) and reflects real-world logistics.
- Timing: Mean onset-to-drug ~100 minutes (SD ~22), consistent with the mechanistic target (hyperacute expansion); timing heterogeneity still exists, and subgroup effects depended strongly on very early treatment (<90 min).
- Outcome assessment: Primary endpoint (mRS at 180 days) is patient-centred and clinically meaningful; imaging endpoints support biological plausibility but cannot substitute for functional benefit.
- Statistical rigour: Prespecified adaptive interim analyses and stopping rules; adjusted ordinal model prespecified; multiplicity handled via Hochberg step-up for secondary efficacy outcomes, but subgroup and interaction findings remain exploratory, especially after early termination.
Conclusion on Internal Validity: Overall, internal validity is moderate to strong due to robust blinding, objective central imaging reads, and prespecified adaptive monitoring, but is limited by early stopping for futility and the inherently exploratory nature of small subgroup signals.
External Validity
- Population representativeness: Selected hyperacute, moderate-volume ICH (2–60 mL) with limited IVH and GCS ≥8; excludes anticoagulant-related ICH and severe pre-stroke disability, reducing applicability to many real-world ICH presentations.
- System requirements: Benefit (if any) likely depends on ultra-fast pathways (ambulance recognition, rapid CT, and often CTA) and immediate treatment within 90 minutes; such pathways are not universally available.
- Care context: High-resource international sites with stroke-unit/ICU care and IV antihypertensive capability; generalisability to resource-limited settings is constrained.
- Imaging-based selection: CTA spot sign was not required at baseline; widespread implementation of a “spot sign–guided” strategy would require near-universal CTA in hyperacute ICH, which may not be feasible everywhere.
Conclusion on External Validity: External validity is limited to moderate: findings apply most directly to hyperacute, selected spontaneous ICH in systems capable of treatment within 2 hours (and ideally <90 minutes), and are less applicable to the broader, later-presenting ICH population.
Strengths & Limitations
- Strengths:
- Largest randomised trial to date targeting ultra-early (≤2 h) haemostatic therapy in spontaneous ICH.
- Double-blind design with central imaging reads and a patient-centred 180-day functional endpoint.
- Demonstrated biological efficacy (reduced haematoma expansion) while simultaneously quantifying thromboembolic harm.
- Operationally pragmatic across diverse systems including mobile stroke units.
- Limitations:
- Stopped early for futility, limiting power for modest effects and for definitive subgroup conclusions.
- Highly selected population (time window, ICH/IVH thresholds, exclusion of anticoagulant-related ICH), limiting generalisability.
- CTA not required, reducing uniformity of “spot sign” ascertainment and complicating translation to a biomarker-guided strategy.
- Increased early life-threatening thromboembolic events constrain the risk–benefit profile, especially without clear functional benefit.
Interpretation & Why It Matters
-
Clinical implicationEven when administered within 2 hours, rFVIIa should not be adopted for routine spontaneous ICH because it did not improve 180-day functional outcomes and increased early life-threatening thromboembolic events.
-
Mechanistic implicationHaemostatic reduction in expansion of ~3–5 mL was insufficient to translate into functional improvement at a population level, reinforcing that surrogate biological success does not guarantee patient-centred benefit.
-
Pathway implicationPotential benefit may be confined to very small, high-risk-of-ongoing-bleeding phenotypes (very early treatment and/or spot sign), but any future evaluation requires rapid “Code ICH” pathways and biomarker-driven enrichment strategies.
Controversies & Subsequent Evidence
- Surrogate success vs clinical failure: FASTEST reduced haematoma expansion (a mechanistically plausible target) yet remained functionally neutral, echoing the prior FAST phase 3 experience and reinforcing scepticism about relying on haematoma growth as a surrogate endpoint for disability/death.1
- Subgroup signals and multiplicity: The trial (and the accompanying Lancet commentary) emphasised caution: small prespecified subgroups (treatment <90 minutes; CTA spot sign) showed non-significant signals, while exploratory interaction models suggested larger effects in combined “very early + spot sign” phenotypes; these findings remain hypothesis-generating and vulnerable to chance, especially after early termination.32
- Risk–benefit constraint: The increased early life-threatening thromboembolic events limits tolerance for uncertainty; without clear functional benefit, even a modest biological advantage is not clinically acceptable.
- How FASTEST fits with other haemostatic strategies: Trials of tranexamic acid in ICH (broad and spot-sign selected) have generally shown limited or no improvement in disability, despite effects on haematoma growth in some contexts, reinforcing the difficulty of converting haemostasis into functional gain.45
- Guidelines and synthesis: Modern evidence syntheses and ICH guidelines continue to recommend against routine haemostatic agent use in spontaneous ICH outside specific indications/trials, reflecting uncertain clinical benefit and potential harms; the 2025 ESO/EANS guideline summarises the totality of evidence across haemostatic interventions.67
- Systems-level subsequent evidence: Pooled analyses support that time-sensitive, bundled care (notably early blood pressure lowering) yields functional benefit in acute ICH, highlighting that “time matters” in ICH, but that the modifiable target might be physiological control rather than haemostasis for most patients.8
- Implementation challenge: Commentaries argue that demonstrating benefit in ultra-early, actively bleeding ICH phenotypes would require reliable prehospital-to-hospital pathways (Code ICH) with rapid CT/CTA and protocolised bundles; without this, global generalisability would be minimal.9
Summary
- FASTEST tested rFVIIa 80 μg/kg (max 10 mg) within 2 hours for spontaneous ICH in a large, international, double-blind phase 3 design.
- Stopped early for futility after 626/860 randomised; no improvement in 180-day functional outcome (adj common OR 1.09; 95% CI 0.79–1.51; P=0.61).
- Haematoma growth was reduced (ICH −3.68 mL; ICH+IVH −5.23 mL), confirming biological haemostasis.
- Life-threatening thromboembolic events within 4 days were increased (RR 3.41; 95% CI 1.14–10.15).
- Subgroup signals (very early treatment and/or spot sign) are hypothesis-generating and require enriched future trials and rapid Code ICH pathways.
Further Reading
Other Trials
- 2005Mayer SA, Brun NC, Begtrup K, et al. Recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2005;352(8):777-785.
- 2008Mayer SA, Brun NC, Begtrup K, et al. Efficacy and safety of recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2008;358(20):2127-2137.
- 2018Sprigg N, Flaherty K, Appleton JP, et al. Tranexamic acid for hyperacute primary intracerebral haemorrhage (TICH-2): an international randomised, placebo-controlled, phase 3 superiority trial. Lancet. 2018;391(10135):2107-2115.
- 2020Meretoja A, Churilov L, Campbell BCV, et al. Tranexamic acid in patients with intracerebral haemorrhage (STOP-AUST): a multicentre, randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2020;19(12):980-987.
- 2016Baharoglu MI, Cordonnier C, Al-Shahi Salman R, et al. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial. Lancet. 2016;387(10038):2605-2613.
Systematic Review & Meta Analysis
Observational Studies
- 2018Morotti A, Boulouis G, Charidimou A, et al. Integration of computed tomographic angiography spot sign and noncontrast computed tomographic hypodensities to predict hematoma expansion. Stroke. 2018;49(9):2067-2073.
- 2020Yogendrakumar V, Ramsay T, Fergusson DA, et al. Redefining hematoma expansion with the inclusion of intraventricular hemorrhage growth. Stroke. 2020;51:1120-1127.
Guidelines
- 2025Steiner T, Purrucker JC, Aguiar de Sousa D, et al. European Stroke Organisation (ESO) and European Association of Neurosurgical Societies (EANS) guideline on stroke due to spontaneous intracerebral haemorrhage. Eur Stroke J. 2025; published online May 22.
- 2021Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the Management of Patients With Spontaneous Intracerebral Hemorrhage. Stroke. 2022;53(7):e282-e361.
Notes
- FASTEST demonstrates a consistent “haemostasis without functional gain” pattern for rFVIIa across eras, while quantifying clinically meaningful early thromboembolic harm.
- rFVIIa within 2 hours reduced haematoma growth but did not improve 180-day functional outcome and increased early life-threatening thromboembolic events
- Early stopping for futility limits definitive subgroup inference; any future benefit would require biomarker/time-based enrichment and Code ICH systems
- 1Mayer SA, Brun NC, Begtrup K, et al. Efficacy and safety of recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2008;358(20):2127-2137.
- 2Mayer SA, Davis SM, Skolnick BE, et al. Can a subset of intracerebral hemorrhage patients benefit from hemostatic therapy with recombinant activated factor VII? Stroke. 2009;40(3):833-840.
- 3Anderson CS, Chen C, Al-Shahi Salman R. Testing early haemostatic therapy for acute intracerebral haemorrhage. Lancet. 2026; published online Feb 4.
- 4Sprigg N, Flaherty K, Appleton JP, et al. Tranexamic acid for hyperacute primary intracerebral haemorrhage (TICH-2): an international randomised, placebo-controlled, phase 3 superiority trial. Lancet. 2018;391(10135):2107-2115.
- 5Meretoja A, Churilov L, Campbell BCV, et al. Tranexamic acid in patients with intracerebral haemorrhage (STOP-AUST): a multicentre, randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2020;19(12):980-987.
- 6Eilertsen H, Menon CS, Law ZK, et al. Haemostatic therapies for stroke due to acute, spontaneous intracerebral haemorrhage. Cochrane Database Syst Rev. 2023;10(10):CD005951.
- 7Steiner T, Purrucker JC, Aguiar de Sousa D, et al. European Stroke Organisation (ESO) and European Association of Neurosurgical Societies (EANS) guideline on stroke due to spontaneous intracerebral haemorrhage. Eur Stroke J. 2025; published online May 22.
- 8Wang X, Ren X, Li Q, et al. Effects of blood pressure lowering in relation to time in acute intracerebral haemorrhage: a pooled analysis of the four INTERACT trials. Lancet Neurol. 2025;24(7):571-579.
- 9Li Q, Yakhkind A, Alexandrov AW, et al. Code ICH: A Call to Action. Stroke. 2024;55(2):494-505.
Overall Takeaway
FASTEST is a landmark ultra-early haemostatic trial in spontaneous ICH because it tested rFVIIa within 2 hours at scale, confirmed a meaningful reduction in haematoma expansion, and demonstrated that this biological effect did not translate into improved disability-free survival while increasing early life-threatening thromboembolic events. It reinforces that haemostatic benefit alone is insufficient for routine adoption and that any future efficacy signal is most plausibly confined to tightly enriched, actively bleeding phenotypes deliverable only within highly optimised hyperacute care pathways.